Mammogram
Mammography; Breast cancer - mammography; Breast cancer - screening mammography; Breast lump - mammogram; Breast tomosynthesis; 3D mammography; 2D mammography; Diagnostic mammogramA mammogram is an x-ray picture of the breasts. It is used to evaluate some breast symptoms and to find breast cancer in women with no symptoms (called screening for breast cancer).
x-ray
X-rays are a type of electromagnetic radiation, just like visible light. An x-ray machine sends individual x-ray waves through the body. The images...

Breast cancer
Breast cancer is cancer that starts in the tissues of the breast. There are two main types of breast cancer:Ductal carcinoma starts in the tubes (du...

How the Test is Performed
You will be asked to undress from the waist up. You will be given a gown to wear. Depending on the type of equipment used and your physical condition, you will sit or stand.
One breast at a time is rested on a flat surface that contains the x-ray plate. A device called a compressor will be pressed firmly against your breast to help flatten the breast tissue. This enables the radiologist to make a better evaluation of your breasts.
The x-ray pictures are taken from several angles. You may be asked to hold your breath as each picture is taken.
You may be asked to come back at a later date to do more mammogram images. This does not always mean you have breast cancer. Your health care provider may simply need to recheck an area that could not be clearly seen on the first test.
TYPES OF MAMMOGRAPHY
Traditional mammography uses film, similar to other x-rays.
Digital mammography is the most common technique:
- It is now used in most breast imaging centers.
- It allows the x-ray image of the breast to be viewed and manipulated on a computer screen.
- It may be more accurate in younger women with dense breasts. It has not yet been proven to help reduce a woman's risk of dying of breast cancer compared to film mammography.
Three-dimensional (3D) mammography (breast tomosynthesis) is a type of digital mammography.
How to Prepare for the Test
Do not use deodorant, perfume, powders, or ointments under your arms or on your breasts on the day of the mammogram. These substances may hide a portion of the images or produce an artifact that can falsely look like an abnormality. Remove all jewelry from your neck and chest area.
Tell your provider and the x-ray technologist if you are pregnant or breastfeeding, or if you've had a breast biopsy.
How the Test will Feel
The compressor surfaces may feel cold. When the breast is pressed down, you may feel some brief pain or discomfort. This needs to be done to get good quality images.
Why the Test is Performed
When and how often to have a screening mammogram is a choice you must make. Different expert groups do not fully agree on the best timing for this test.
Before having a mammogram, talk to your provider about the pros and cons of having the test. Ask about:
- Your risk for breast cancer
Risk for breast cancer
Breast cancer risk factors are things that increase the chance that you could get cancer. Some risk factors you can control, such as drinking alcoho...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Whether screening decreases your chance of dying from breast cancer
- Whether there is any harm from breast cancer screening, such as side effects from testing or overtreatment of cancer when it's discovered
Mammography is performed to screen women to detect early breast cancer when it is more likely to be cured. The recommendations of different expert organizations can differ.
- Mammography is generally recommended for all women starting at age 40, repeated every 1 to 2 years.
- Women with a family history of breast cancer should work with their provider to assess their risk of breast cancer. In some situations, additional testing may be considered.
Mammograms work best at finding breast cancer in women ages 40 to 74. It is not clear how well mammograms work at finding cancer in women age 75 and older.
Mammography is also used to:
- Follow a woman who has had an abnormal mammogram.
- Evaluate a woman who has symptoms of a breast disease. These symptoms may include a lump, nipple discharge, breast pain, dimpling of the skin on the breast, changes of the nipple, or other findings.
Breast pain
Breast pain is any discomfort or pain in the breast.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Normal Results
Breast tissue that shows no signs of a mass or suspicious looking calcifications is considered normal.
Calcifications
Calcifications are tiny deposits of calcium in your breast tissue. They are often seen on a mammogram.

What Abnormal Results Mean
Most abnormal findings on a screening mammogram turn out to be benign (not cancer) or nothing to worry about. New findings or changes must be further evaluated.
A radiology specialist (radiologist) may see the following types of findings on a mammogram:
- A well-outlined, smoothly marginated, rounded spot (this is more likely to be a noncancerous condition, such as a cyst)
Cyst
A cyst is a closed pocket or pouch of tissue. It can be filled with air, fluid, pus, or other material.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Irregular appearing masses or lumps
- Dense areas in the breast that can be breast cancer or hide breast cancer
- Calcifications, which are caused by tiny deposits of calcium in the breast tissue (most calcifications are not a sign of cancer)
At times, the following tests are also needed to further assess mammogram findings:
- Additional mammogram views, including magnification or compression views
- Breast ultrasound
Breast ultrasound
Breast ultrasound is a test that uses sound waves to examine the breasts.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Breast MRI exam (less commonly done)
Breast MRI exam
A breast MRI scan is an imaging test that uses powerful magnets and radio waves to create pictures of the breast and surrounding tissue. It does not...
Read Article Now Book Mark Article
Comparing your current mammogram to your past mammograms helps the radiologist tell whether you had an abnormal finding in the past and whether it has changed.
When mammogram or ultrasound results look suspicious, a biopsy is done to test the tissue and see if it is cancerous. Types of biopsies include:
Biopsy
A biopsy is the removal of a small piece of tissue for lab examination.

- Stereotactic (guided)
Stereotactic
A breast biopsy is the removal of breast tissue to examine it for signs of breast cancer or other disorders. There are several types of breast biops...
Read Article Now Book Mark Article - Ultrasound (guided)
Ultrasound
A breast biopsy is the removal of breast tissue to examine it for signs of breast cancer or other disorders. There are several types of breast biopsi...
Read Article Now Book Mark Article - Open (surgical)
Open (surgical)
Breast lump removal is surgery to remove a lump that may be a breast cancer. Tissue around the lump is also removed. This surgery is called an exci...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks
The level of radiation is low and any risk from mammography is very low. If you are pregnant and need to have an abnormality checked, your belly area will be covered and protected by a lead apron.
Routine screening mammography is not done during pregnancy or while breastfeeding.
References
Allweis TM, Grubstein A, Menes T. Breast cancer screening. In: Klimberg VS, Gradishar WJ, Bland KI, Korourian S, White J, Copeland EM, eds. Bland and Copeland's The Breast: Comprehensive Management of Benign and Malignant Diseases. 6th ed. Philadelphia, PA: Elsevier; 2024:chap 12.
American Cancer Society website. American Cancer Society recommendations for the early detection of breast cancer. www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html. Revised December 19, 2023. Accessed January 27, 2025.
American College of Obstetrics and Gynecology. Age to initiate routine breast cancer screening. ACOG Clinical Practice Update. Obstet Gynecol. 2025;145(1):e40-e44. PMID: 39388713 pubmed.ncbi.nlm.nih.gov/39388713/.
Henry NL, Shah PD, Haider I, Freer PE, Jagsi R, Sabel MS. Cancer of the breast. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 88.
National Cancer Institute website. Breast cancer screening (PDQ) - health professional version. www.cancer.gov/types/breast/hp/breast-screening-pdq. Updated October 9, 2024. Accessed January 27, 2025.
US Preventive Services Task Force; Nicholson WK, Silverstein M, et al. Screening for breast cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2024;331(22):1918-1930. PMID: 38687503 pubmed.ncbi.nlm.nih.gov/38687503/.
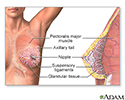
Female Breast - illustration
The female breast is either of two mammary glands (organs of milk secretion) on the chest.
Female Breast
illustration
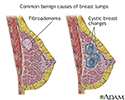
Breast lumps - illustration
Less than one-fourth of all breast lumps are found to be cancerous, but benign breast disease can be difficult to distinguish from cancer. Consequently, all breast lumps should be checked by a health care professional. Imaging tests such as mammogram and ultrasound may be needed for evaluation.
Breast lumps
illustration
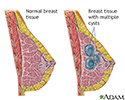
Causes of breast lumps - illustration
Most breast lumps are benign (non-cancerous), as in fibroadenoma, a condition that mostly affects women under age 30. Fibrocystic breast changes occur in more than 60% of all women. Fibrocystic breast cysts change in size with the menstrual cycle, whereas a lump from fibroadenoma does not. While most breast lumps are benign, it is important to identify those that are not. See your health care provider if a lump is new, persistent, growing, hard, immobile, or causing skin deformities.
Causes of breast lumps
illustration
Mammary gland - illustration
The anatomy of the breast includes the lactiferous, or milk ducts, and the mammary lobules.
Mammary gland
illustration
Abnormal discharge from the nipple - illustration
Abnormal nipple discharge may be described as any discharge not associated with lactation. The nature of the discharge may range in color, consistency and composition, and occur in one or both breasts.
Abnormal discharge from the nipple
illustration
Fibrocystic breast disease - illustration
Fibrocystic breast change is a common and benign change within the breast characterized by a dense irregular and bumpy consistency in the breast tissue. Mammography or biopsy may be needed to rule out other disorders.
Fibrocystic breast disease
illustration
Mammogram - illustration
A mammogram is an x-ray picture of the breasts. It is used to find tumors and to help tell the difference between noncancerous (benign) and cancerous (malignant) disease. One breast at a time is rested on a flat surface that contains the x-ray plate. A device called a compressor is pressed firmly against the breast to help flatten out the breast tissue. Each breast is compressed horizontally, then obliquely and an x-ray is taken of each position.
Mammogram
illustration
Female Breast - illustration
The female breast is either of two mammary glands (organs of milk secretion) on the chest.
Female Breast
illustration
Breast lumps - illustration
Less than one-fourth of all breast lumps are found to be cancerous, but benign breast disease can be difficult to distinguish from cancer. Consequently, all breast lumps should be checked by a health care professional. Imaging tests such as mammogram and ultrasound may be needed for evaluation.
Breast lumps
illustration
Causes of breast lumps - illustration
Most breast lumps are benign (non-cancerous), as in fibroadenoma, a condition that mostly affects women under age 30. Fibrocystic breast changes occur in more than 60% of all women. Fibrocystic breast cysts change in size with the menstrual cycle, whereas a lump from fibroadenoma does not. While most breast lumps are benign, it is important to identify those that are not. See your health care provider if a lump is new, persistent, growing, hard, immobile, or causing skin deformities.
Causes of breast lumps
illustration
Mammary gland - illustration
The anatomy of the breast includes the lactiferous, or milk ducts, and the mammary lobules.
Mammary gland
illustration
Abnormal discharge from the nipple - illustration
Abnormal nipple discharge may be described as any discharge not associated with lactation. The nature of the discharge may range in color, consistency and composition, and occur in one or both breasts.
Abnormal discharge from the nipple
illustration
Fibrocystic breast disease - illustration
Fibrocystic breast change is a common and benign change within the breast characterized by a dense irregular and bumpy consistency in the breast tissue. Mammography or biopsy may be needed to rule out other disorders.
Fibrocystic breast disease
illustration
Mammogram - illustration
A mammogram is an x-ray picture of the breasts. It is used to find tumors and to help tell the difference between noncancerous (benign) and cancerous (malignant) disease. One breast at a time is rested on a flat surface that contains the x-ray plate. A device called a compressor is pressed firmly against the breast to help flatten out the breast tissue. Each breast is compressed horizontally, then obliquely and an x-ray is taken of each position.
Mammogram
illustration
Review Date: 1/15/2025
Reviewed By: Kenneth Levin, MD, Private Practice specializing in Radiology and Nuclear Medicine, Allentown, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.