Breast lump removal
Lumpectomy; Wide local excision; Breast conservation surgery; Breast-sparing surgery; Partial mastectomy; Segmental resection; TylectomyBreast lump removal is surgery to remove a lump that may be a breast cancer. Tissue around the lump is also removed. This surgery is called an excisional breast biopsy, or lumpectomy.
When a noncancerous tumor such as a fibroadenoma of the breast is removed, this is also called an excisional breast biopsy, or a lumpectomy.
Fibroadenoma
Fibroadenoma of the breast is a benign tumor. Benign tumor means it is not a cancer.
Description
Sometimes, the health care provider cannot feel the lump when examining you. However, it can be seen on imaging results, such as a mammogram or ultrasound. In this case, a wire localization will be done before the surgery.
- A radiologist will use a mammogram or ultrasound to place a needlewire (or needlewires) in or near the abnormal breast area.
Mammogram
A mammogram is an x-ray picture of the breasts. It is used to evaluate some breast symptoms and to find breast cancer in women with no symptoms (cal...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleUltrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - This will help the surgeon know where the lump is so that it can be removed.
Breast lump removal is done as an outpatient surgery most of the time. You will be given general anesthesia (you will be asleep, but pain free) or local anesthesia (you are lightly sedated and pain free). The procedure takes about 1 hour.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
The surgeon makes a small cut on your breast. The lump and some of the normal breast tissue around it is removed. If a lump is known to be cancerous, a pathologist examines a sample of the removed tissue to make sure all the cancer has been taken out.
- When no cancer cells are found near the edges of the removed tissue, it is called a clear margin.
- Your surgeon may also remove some or all of the lymph nodes in your armpit to see if the cancer has spread to them.
Often, small metal clips will be placed inside the breast to mark the area of tissue removal, especially if there is a concern for cancer. This makes the area easy to see on future mammograms. It also helps guide radiation therapy, when needed.
The surgeon will close your skin with stitches or staples. These may dissolve or need to be removed later. Rarely, a drain tube may be placed to remove extra fluid. Your surgeon will send the lump to the pathologist for more testing.
Why the Procedure Is Performed
Surgery to remove a breast cancer is most often the first step in treatment.
Breast cancer
Breast cancer is cancer that starts in the tissues of the breast. There are two main types of breast cancer:Ductal carcinoma starts in the tubes (du...

The choice of which surgery is best for you can be difficult. It may be hard to know whether lumpectomy or mastectomy (removal of the entire breast) is best. You and the providers who are treating your breast cancer will decide together. In general:
- Lumpectomy is often preferred for smaller breast lumps. This is because it is a smaller procedure and it has about the same chance of curing breast cancer as a mastectomy. It is a good option as you get to keep most of your breast tissue that has not been affected by cancer.
Breast lumps
A breast lump is swelling, growth, or mass in the breast. Breast lumps in both men and women raise concern for breast cancer, even though most lumps...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMastectomy
A mastectomy is surgery to remove the breast tissue. Some of the skin and the nipple may also be removed. The surgery is most often done to treat b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Mastectomy to remove all breast tissue may be done if the area of cancer is too large or there are multiple tumors which cannot be removed without deforming the breast.
You and your provider should consider:
- The size of your tumor
- Where it is in your breast
- If there is more than one tumor
- How much of the breast is affected
- The size of your breasts in relation to the tumor
- Your age
- Your family history
- Your general health, including whether you have reached menopause
- If you are pregnant
- If you are not a candidate for additional treatment such as radiation
Risks
Risks for surgery are:
- Bleeding
Bleeding
Bleeding is the loss of blood. Bleeding may be:Inside the body (internal)Outside the body (external)Bleeding may occur:Inside the body when blood le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infection
- Poor wound healing
- Heart attack, stroke, death
Heart attack
Most heart attacks are caused by a blood clot that blocks one of the coronary arteries. The coronary arteries bring blood and oxygen to the heart. ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleStroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Reactions to medicines
- Risks associated with general anesthesia
The appearance of your breast may change after surgery. You may notice dimpling, a scar, or a difference in shape between your breasts. Also, areas of the breast may be numb, such as near the scar, or the nipple.
You may need another procedure to remove more breast tissue if tests show the cancer is too close to the edge of the tissue already removed.
Before the Procedure
Always tell your provider:
- If you could be pregnant
- What medicines you are taking, even medicines or herbs you bought without a prescription
- Any allergies you may have, including medicines, foods and latex or rubber
- Reactions to anesthesia in the past
During the days before your surgery:
- You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), clopidogrel (Plavix), warfarin (Coumadin), and any other medicines that make it hard for your blood to clot. Be sure to ask your surgeon which medicines should be stopped, and for how long before your procedure.
- Ask your provider which medicines you should still take on the day of your surgery.
- If you smoke, try to stop for at least 2 weeks prior to the surgery. Your provider can help.
On the day of surgery:
- Follow your provider's instructions about eating or drinking before surgery.
- Take the medicines your provider told you to take with a small sip of water.
- Your provider will tell you when to arrive for the procedure.
After the Procedure
The recovery period is very short for a simple lumpectomy. Many women have little pain, but if you do feel pain, you can take pain medicine, such as acetaminophen.
Your skin should heal in about a month. You will need to take care of the surgical cut area. Change dressings as your provider tells you to. Watch for signs of infection when you get home (such as redness, swelling, or drainage from the incision). Wear a comfortable bra that provides good support, such as a sports bra. You may need to put some gauze over the incision so that the bra does not irritate it.
Take care of the surgical cut area
An incision is a cut through the skin that is made during surgery. It is also called a surgical wound. Some incisions are small, others are long. ...

You may need to empty a fluid drain a few times a day for 1 to 2 weeks. You may be asked to measure and record the amount of fluid drained. Your provider will remove the drain later.
Most women can go back to their usual activities in a week or so. Avoid heavy lifting, jogging, or activities that cause pain in the surgical area for 1 to 2 weeks. Check with your surgeon prior to driving, or going back to work.
Outlook (Prognosis)
The outcome of a lumpectomy for breast cancer depends mostly on the size of the cancer, as well as the make up of the tumor. It also depends on its spread to lymph nodes underneath your arm.
A lumpectomy for breast cancer is most often followed by radiation therapy and other treatments such as chemotherapy, hormonal therapy, or both.
Radiation therapy
Radiation therapy uses high-powered radiation (such as x-rays or gamma rays), particles, or radioactive seeds to kill cancer cells.

Chemotherapy
The term chemotherapy is used to describe cancer-killing drugs. Chemotherapy may be used to:Cure the cancerShrink the cancerPrevent the cancer from ...

Hormonal therapy
Hormone therapy (HT) uses one or more hormones to treat symptoms of menopause. HT uses estrogen, progestin (a type of progesterone), or both. Somet...
In most cases, you do not need a breast reconstruction after lumpectomy.
Breast reconstruction
After a mastectomy, some women choose to have surgery to rebuild their breast. This type of surgery is called breast reconstruction. It can be perf...
References
American Cancer Society website. Breast-conserving surgery (lumpectomy). www.cancer.org/cancer/types/breast-cancer/treatment/surgery-for-breast-cancer/breast-conserving-surgery-lumpectomy. Updated October 27, 2021. Accessed November 6, 2024.
American Society of Breast Surgeons. Performance and practice guidelines for breast-conserving surgery/partial mastectomy. www.breastsurgeons.org/docs/statements/Performance-and-Practice-Guidelines-for-Breast-Conserving-Surgery-Partial-Mastectomy.pdf. Updated February 22, 2015. Accessed November 6, 2024.
Gladden AAH, Finlayson CA. Early breast cancer. In: McIntyre RC, Schulick RD, eds. Surgical Decision Making. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 101.
Henry NL, Shah PD, Haider I, Freer PE, Jagsi R, Sabel MS. Cancer of the breast. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 88.
Klimberg VS, Hunt KK. Diseases of the breast. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 35.
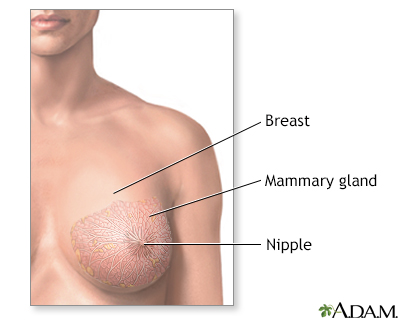
Female Breast - illustration
The female breast is either of two mammary glands (organs of milk secretion) on the chest.
Female Breast
illustration
Open biopsy of the breast - illustration
An open biopsy can be performed under local or general anesthesia and will leave a small scar. Prior to surgery, a radiologist often first marks the lump with a wire, making it easier for the surgeon to find.
Open biopsy of the breast
illustration
Breast self-exam - illustration
Monthly breast self-exams should always include a visual inspection, with and without a mirror, to note any changes in contour or texture, and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Breast self-exam
illustration
Breast self-exam - illustration
Monthly breast self-exams should always include a visual inspection, with and without a mirror, to note any changes in contour or texture, and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Breast self-exam
illustration
Breast self-exam - illustration
Monthly breast self-exams should always include a visual inspection, with and without a mirror, to note any changes in contour or texture, and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Breast self-exam
illustration
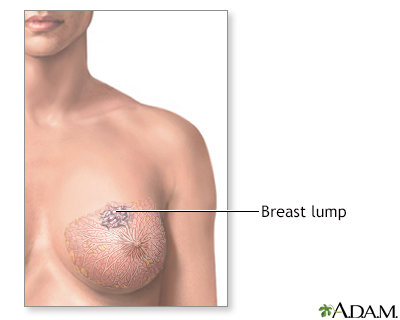
Breast lumps - illustration
Less than one-fourth of all breast lumps are found to be cancerous, but benign breast disease can be difficult to distinguish from cancer. Consequently, all breast lumps should be checked by a health care professional. Imaging tests such as mammogram and ultrasound may be needed for evaluation.
Breast lumps
illustration
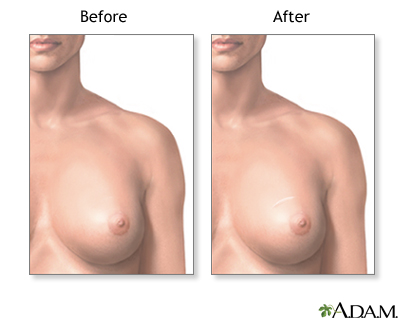
Lumpectomy - illustration
Lumpectomy is a surgical procedure performed on a solid breast mass to determine if it is malignant. The suspicious lump and some surrounding tissue is excised and analyzed.
Lumpectomy
illustration
Causes of breast lumps - illustration
Most breast lumps are benign (non-cancerous), as in fibroadenoma, a condition that mostly affects women under age 30. Fibrocystic breast changes occur in more than 60% of all women. Fibrocystic breast cysts change in size with the menstrual cycle, whereas a lump from fibroadenoma does not. While most breast lumps are benign, it is important to identify those that are not. See your health care provider if a lump is new, persistent, growing, hard, immobile, or causing skin deformities.
Causes of breast lumps
illustration
Breast lump removal - series - Normal anatomy
Presentation
Core needle biopsy of the breast - illustration
A core needle biopsy of the breast is a procedure to remove samples of tissue from a lump or suspicious area of the breast and evaluate it for breast cancer. Core needle biopsy uses a long, hollow needle to take several core samples of tissue, usually using ultrasound or mammographic guidance. The samples are then sent to a lab for analysis.
Core needle biopsy of the breast
illustration
Female Breast - illustration
The female breast is either of two mammary glands (organs of milk secretion) on the chest.
Female Breast
illustration
Open biopsy of the breast - illustration
An open biopsy can be performed under local or general anesthesia and will leave a small scar. Prior to surgery, a radiologist often first marks the lump with a wire, making it easier for the surgeon to find.
Open biopsy of the breast
illustration
Breast self-exam - illustration
Monthly breast self-exams should always include a visual inspection, with and without a mirror, to note any changes in contour or texture, and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Breast self-exam
illustration
Breast self-exam - illustration
Monthly breast self-exams should always include a visual inspection, with and without a mirror, to note any changes in contour or texture, and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Breast self-exam
illustration
Breast self-exam - illustration
Monthly breast self-exams should always include a visual inspection, with and without a mirror, to note any changes in contour or texture, and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Breast self-exam
illustration
Breast lumps - illustration
Less than one-fourth of all breast lumps are found to be cancerous, but benign breast disease can be difficult to distinguish from cancer. Consequently, all breast lumps should be checked by a health care professional. Imaging tests such as mammogram and ultrasound may be needed for evaluation.
Breast lumps
illustration
Lumpectomy - illustration
Lumpectomy is a surgical procedure performed on a solid breast mass to determine if it is malignant. The suspicious lump and some surrounding tissue is excised and analyzed.
Lumpectomy
illustration
Causes of breast lumps - illustration
Most breast lumps are benign (non-cancerous), as in fibroadenoma, a condition that mostly affects women under age 30. Fibrocystic breast changes occur in more than 60% of all women. Fibrocystic breast cysts change in size with the menstrual cycle, whereas a lump from fibroadenoma does not. While most breast lumps are benign, it is important to identify those that are not. See your health care provider if a lump is new, persistent, growing, hard, immobile, or causing skin deformities.
Causes of breast lumps
illustration
Breast lump removal - series - Normal anatomy
Presentation
Core needle biopsy of the breast - illustration
A core needle biopsy of the breast is a procedure to remove samples of tissue from a lump or suspicious area of the breast and evaluate it for breast cancer. Core needle biopsy uses a long, hollow needle to take several core samples of tissue, usually using ultrasound or mammographic guidance. The samples are then sent to a lab for analysis.
Core needle biopsy of the breast
illustration
Review Date: 10/17/2024
Reviewed By: Linda J. Vorvick, MD, Clinical Professor, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.