Familial Mediterranean fever
Familial paroxysmal polyserositis; Periodic peritonitis; Recurrent polyserositis; Benign paroxysmal peritonitis; Periodic disease; Periodic fever; FMFFamilial Mediterranean fever (FMF) is a rare disorder that may be passed down through families (inherited). It involves repeated fevers and inflammation that often affects the lining of the abdomen, chest, or joints.
Causes
FMF is most often caused by a variation in a gene named MEFV. This gene creates a protein involved in regulating inflammation. The disease usually appears only in people who received two copies of the variant gene, one from each parent. This is called autosomal recessive inheritance or an autosomal recessive condition.
FMF most often affects people of Mediterranean ancestry. These include non-Ashkenazi (Sephardic) Jews, Armenians, and Arabs. People from other ethnic groups can also be affected.
Symptoms
Symptoms usually begin between ages 5 and 15. Inflammation in the lining of the abdominal cavity, chest cavity, skin, or joints occurs along with high fevers that usually peak in 12 to 24 hours. Attacks may vary in severity of symptoms. People are usually symptom-free between attacks.
Symptoms may include repeated episodes of:
- Abdominal pain
Abdominal pain
Abdominal pain is pain that you feel anywhere between your chest and groin. This is often referred to as the stomach region or belly.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chest pain that is sharp and gets worse when taking a breath
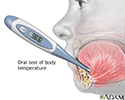
- Fever or alternating chills and fever
- Joint pain
- Skin sores (lesions) that are red and swollen and range from 5 to 20 centimeters (cm) in diameter
Exams and Tests
If genetic testing shows that you have two pathogenic variants and your symptoms match the typical pattern, the diagnosis is nearly certain. Lab tests and x-rays or other imaging tests are used to check for other possible diseases to help confirm the diagnosis.
x-rays
X-rays are a type of electromagnetic radiation, just like visible light. An x-ray machine sends individual x-ray waves through the body. The images...

Levels of certain blood tests may be higher than normal when done during an attack. Tests may include:
- Complete blood count (CBC) that includes white blood cell count
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - C-reactive protein (CRP) to check for inflammation
C-reactive protein
C-reactive protein (CRP) is produced by the liver. The level of CRP rises when there is inflammation in the body. It is one of a group of proteins,...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Erythrocyte sedimentation rate (ESR) to check for inflammation
Erythrocyte sedimentation rate
ESR stands for erythrocyte sedimentation rate. It is commonly called a "sed rate. "It is a test that indirectly measures the level of certain protei...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fibrinogen test to check blood clotting
Fibrinogen test
Fibrinogen is a protein produced by the liver. This protein helps stop bleeding by helping blood clots to form. A blood test can be done to tell ho...
Read Article Now Book Mark Article
Treatment
The goal of treatment for FMF is to regulate symptoms. Colchicine, a medicine that reduces inflammation, may help during an attack and may prevent further attacks. It can also help prevent a serious complication called systemic amyloidosis, which is common in people with FMF.
Amyloidosis
Primary amyloidosis is a rare disorder in which abnormal proteins build up in tissues and organs. Clumps of the abnormal proteins are called amyloid...

Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to treat fever and pain.
Outlook (Prognosis)
There is no known cure for FMF. Most people continue to have attacks, but the number and severity of attacks is different from person to person.
Possible Complications
Amyloidosis may lead to kidney damage or not being able to absorb nutrients from food (malabsorption). Fertility problems in women and men and arthritis are also complications.
When to Contact a Medical Professional
Contact your health care provider if you or your child develops symptoms of this condition.
References
Assady S, Ramadan R, Frishberg Y. Near and middle east. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 78.
Kastner DL. The systemic autoinflammatory diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 240.
Verbsky JW. Hereditary periodic fever syndromes and other systemic autoinflammatory diseases. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 204.
Review Date: 8/18/2024
Reviewed By: Anna C. Edens Hurst, MD, MS, Associate Professor in Medical Genetics, The University of Alabama at Birmingham, Birmingham, AL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.